Dental Insurance Accepted Practices in Queens: Maximizing Your Benefits
When maneuvering through dental insurance in Queens, understanding accepted practices is essential for maximizing benefits. Identifying in-network dentists guarantees minimal out-of-pocket expenses, while thorough understanding of policy details aids in securing all-inclusive preventive care coverage. Engaging with dental offices for cost-saving strategies on major procedures can further optimize insurance usage. Utilizing tools like Flexible Spending Accounts for eligible expenses offers additional financial advantages. Explore these strategies to manage dental costs effectively.
Understanding Dental Insurance Basics
When delving into the fundamentals of dental insurance, it is essential for patients to comprehend the key concepts that define this specialized form of coverage. A thorough understanding of dental policy terms is vital for maneuvering the complexities of coverage limitations, annual maximums, and deductible requirements. Patients should familiarize themselves with terms such as “premium,” “co-payment,” and “waiting period” to avoid unexpected expenses.
The insurance claim processes also play a significant role in maximizing benefits. This involves submitting accurate documentation and understanding pre-authorization procedures, which can expedite claim approvals. Patients must be diligent in tracking claim statuses and ensuring all necessary forms are completed correctly. By grasping these essential elements, patients can adeptly manage their dental insurance, ensuring ideal utilization of their benefits.
Types of Dental Insurance Plans Available
Although dental insurance can be complex, understanding the different types of plans available is essential for patients looking to make informed decisions about their oral health coverage. Preferred Provider Organization (PPO) Plans offer flexibility, allowing patients to visit any dentist but providing greater benefits when selecting in-network providers. Health Maintenance Organization (HMO) Plans require patients to choose a primary care dentist within the network, offering lower premiums and no deductibles, but limiting provider choice. Indemnity Plans, often referred to as traditional insurance, provide the freedom to visit any dentist, with reimbursement based on a predetermined fee schedule. Discount Plans, while not insurance, offer reduced rates on dental procedures through a network of participating providers, beneficial for patients without extensive insurance coverage.
Finding In-Network Dentists in Queens
Locating in-network dentists in Queens requires accessing the dental networks associated with one’s insurance provider, which guarantees ideal benefit utilization and cost-effectiveness. Patients should meticulously verify their insurance coverage to ascertain the inclusion of specific dental practitioners within their plan. This process not only enhances the efficiency of dental care access but also minimizes unexpected financial liabilities.
Search Dental Networks
To effectively navigate dental insurance options in Queens, it is essential to understand how to locate in-network dentists within various dental networks. Patients can begin by consulting their insurance providers’ online portals or customer service for lists of participating dental professionals. These resources typically offer search functionalities based on location, specialty, and network affiliations. Identifying in-network dentists is critical, as it guarantees patients maximize their benefits while minimizing out-of-pocket expenses. Additionally, insurance providers often update their dental networks periodically, so periodic verification is advisable. Understanding network-specific details, such as covered services and co-payment requirements, empowers patients to make informed decisions. Thorough research and utilization of available resources streamline the process of finding suitable dental care within the extensive networks available in Queens.
Verify Insurance Coverage
When verifying insurance coverage to find in-network dentists in Queens, individuals should prioritize examining the specifics of their dental insurance plans. A thorough understanding of the insurance policy is vital to identify coverage limits and guarantee ideal utilization of benefits. Policyholders must review their plan documents to ascertain which dental services are covered and any restrictions that might apply. Identifying in-network providers is important, as these dentists have pre-negotiated rates, reducing out-of-pocket expenses for patients. Individuals should contact their insurance company directly or visit their website to access an updated directory of participating dentists in Queens. Additionally, confirming any pre-authorization requirements for specific procedures can prevent unforeseen costs. This meticulous approach guarantees that patients maximize their benefits while minimizing financial surprises.
Evaluating Coverage for Preventive Care
Evaluating coverage for preventive care in dental insurance requires a thorough understanding of what constitutes preventive services, such as biannual cleanings, routine check-ups, and fluoride treatments. These services are often covered with little to no out-of-pocket cost, underscoring their importance in maintaining oral health and preventing more severe dental issues. Patients should thoroughly review their policy details to verify that routine preventive care is fully covered, thereby maximizing their insurance benefits while promoting long-term dental wellness.
Understanding Preventive Coverage
How effectively does preventive dental coverage serve the insured in Queens? Preventive services, such as dental cleanings, fluoride treatments, and sealants, are critical components in maintaining oral health and mitigating future dental issues. Insurance plans often emphasize these services by offering substantial coverage, sometimes up to 100%, to encourage regular dental visits. Understanding coverage limits is paramount; while most plans cover biannual check-ups, additional preventive procedures may require out-of-pocket expenses if they exceed the policy’s predefined limits. Detailed examination of policy documents enables patients to maximize their benefits while minimizing unexpected costs. It is vital for patients to verify the specifics of their plan’s preventive coverage to guarantee thorough care and avoid surpassing allocated coverage limits.
Routine Check-up Benefits
Routine check-up benefits form a cornerstone of preventive dental care, offering patients in Queens a structured pathway to maintain oral health. These benefits underscore the routine check-up significance, which includes biannual examinations and cleanings—a standard preventive care frequency recommended by dental professionals. Insurance plans frequently cover these services at 100%, recognizing their efficacy in early detection of oral health issues, thereby reducing the need for extensive treatments. Evaluating coverage details guarantees patients fully utilize these benefits, understanding that routine visits aid in the removal of plaque and identification of potential problems. Consequently, the financial burden of more complex procedures is mitigated, reinforcing the value of preventive care. Awareness and regular use of these benefits are crucial in optimizing dental health outcomes.
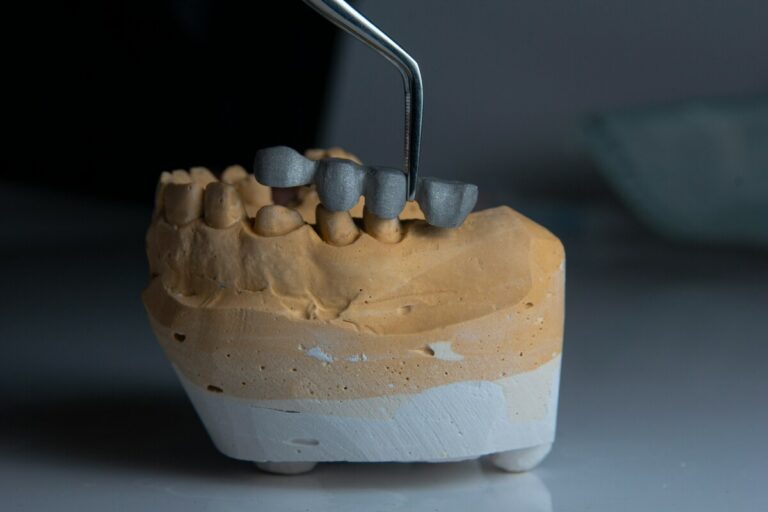
Managing Costs for Major Dental Procedures
Maneuvering the financial landscape of major dental procedures can be challenging, but a strategic approach to managing costs can alleviate much of the burden. Effective cost management involves detailed procedure planning, specifically tailored to the patient’s insurance benefits. Patients should begin by consulting their insurance provider to understand the coverage specifics for major treatments such as crowns, bridges, or implants. In-depth discussions with the dental office can help identify potential cost-saving measures, such as phased treatment plans or alternative materials that maintain quality while reducing expenses. Additionally, exploring in-network provider options can further minimize out-of-pocket costs. By proactively engaging in these strategies, patients can achieve a balance between necessary dental care and financial feasibility.
Tips for Choosing the Right Dentist
Selecting the right dentist involves a meticulous evaluation of several factors to guarantee ideal dental care and patient satisfaction. Initially, reviewing dentist qualifications is paramount. This includes verifying board certification, specialized training, and continued education, which reflect a commitment to clinical excellence. Moreover, examining patient reviews provides insights into the dentist’s proficiency, bedside manner, and office environment, offering a glimpse into other patients’ experiences. Additionally, the practice’s location, office hours, and emergency care options should align with the patient’s logistical needs. Modern technological capabilities, such as digital X-rays and CAD/CAM systems, indicate a forward-thinking practice embracing innovations for enhanced care. Ultimately, a thorough approach to evaluating these elements guarantees a well-informed decision and optimizes dental health outcomes.
Strategies for Maximizing Annual Benefits
Effectively maximizing annual dental insurance benefits requires a strategic and informed approach. Patients should begin by thoroughly reviewing their policy documents to understand coverage limitations and exclusions. Annual benefit strategies include scheduling preventive services, such as cleanings and examinations, early in the year to identify potential issues that might require more extensive treatments. This proactive scheduling guarantees timely insurance claim optimization, allowing for the full utilization of benefits before year’s end. Additionally, patients should prioritize necessary treatments and communicate with their dental provider to plan procedures that align with their coverage limits. By maintaining detailed records of past claims and ongoing treatments, patients can efficiently track their benefit usage, thereby preventing unexpected out-of-pocket expenses and enhancing the overall value of their dental insurance plan.
Navigating Out-of-Network Options
When considering dental care options outside of an insurance network, how can patients make informed decisions? Understanding out of network costs is vital. Patients should request a detailed fee schedule from potential providers to compare with in-network rates. An essential step is verifying the insurance reimbursement policy for out-of-network services by contacting the insurance company directly. Some plans offer partial reimbursement, while others may not cover certain procedures at all. Patients should review their Explanation of Benefits (EOB) to assess coverage specifics. Calculating the financial impact, including potential higher out-of-pocket expenses, enables informed decision-making. Additionally, patients can inquire if providers offer payment plans or discounts for out-of-network procedures, optimizing cost management while ensuring access to necessary dental care.
Utilizing Flexible Spending Accounts for Dental Care
How can patients enhance their dental care expenses using Flexible Spending Accounts (FSAs)? FSAs allow individuals to allocate pre-tax dollars for qualified medical expenses, including dental expenses, thereby reducing taxable income. According to IRS guidelines, these expenses encompass preventive care, fillings, extractions, and orthodontics. Patients in Queens can benefit by strategically planning dental procedures within the FSA plan year to guarantee ideal utilization. Key considerations include the “use-it-or-lose-it” rule, requiring funds to be spent by year-end or they are forfeited. In addition, aligning larger dental procedures with FSA contributions can substantially alleviate out-of-pocket costs. Patients should consult their dental practice to confirm the eligibility of specific treatments under FSA provisions, thereby maximizing financial benefits through strategic flexible spending.
Frequently Asked Questions
Can Dental Insurance Cover Cosmetic Procedures Like Teeth Whitening?
Dental insurance typically excludes cosmetic coverage for procedures like teeth whitening, considering them elective rather than medically necessary. Whitening limitations often apply, as insurers prioritize restorative or preventive treatments, underscoring the importance of reviewing individual policy details.
How Do Emergency Dental Visits Work With Insurance?
Emergency dental visits function under insurance through emergency coverage provisions. Urgent care is often prioritized, and insurance policies may cover necessary treatments. Patients should verify specific terms and limits with their provider to guarantee adequate coverage.
Are There Waiting Periods for New Dental Insurance Plans?
Waiting period policies for new dental insurance plans often vary, typically involving a delay before plan activation allows coverage for certain procedures. It is essential for patients to review specific terms to understand coverage commencement and benefits eligibility.
Do Dental Insurance Plans Cover Orthodontic Treatments Like Braces?
Orthodontic coverage typically varies among dental insurance plans, with braces eligibility often subject to specific policy terms. Patients should review their plan’s details, focusing on age restrictions and lifetime maximums, to understand their orthodontic treatment benefits accurately.
How Does Dental Insurance Coordinate With Other Health Insurance Benefits?
Dental insurance coordinates with other health insurance benefits through coordination benefits, ensuring that claims are processed correctly. This involves maneuvering through insurance networks to determine primary and secondary coverage, optimizing cost-sharing, and preventing overlapping payments for patient care.